During this 20-25 minute pre-recorded lecture, Dr. Pascale M. White discusses the topic of celiac disease. This in-depth review will provide an update on this topic for your clinical practice as well as supplement your learning for the ABIM Gastroenterology and Hepatology boards.
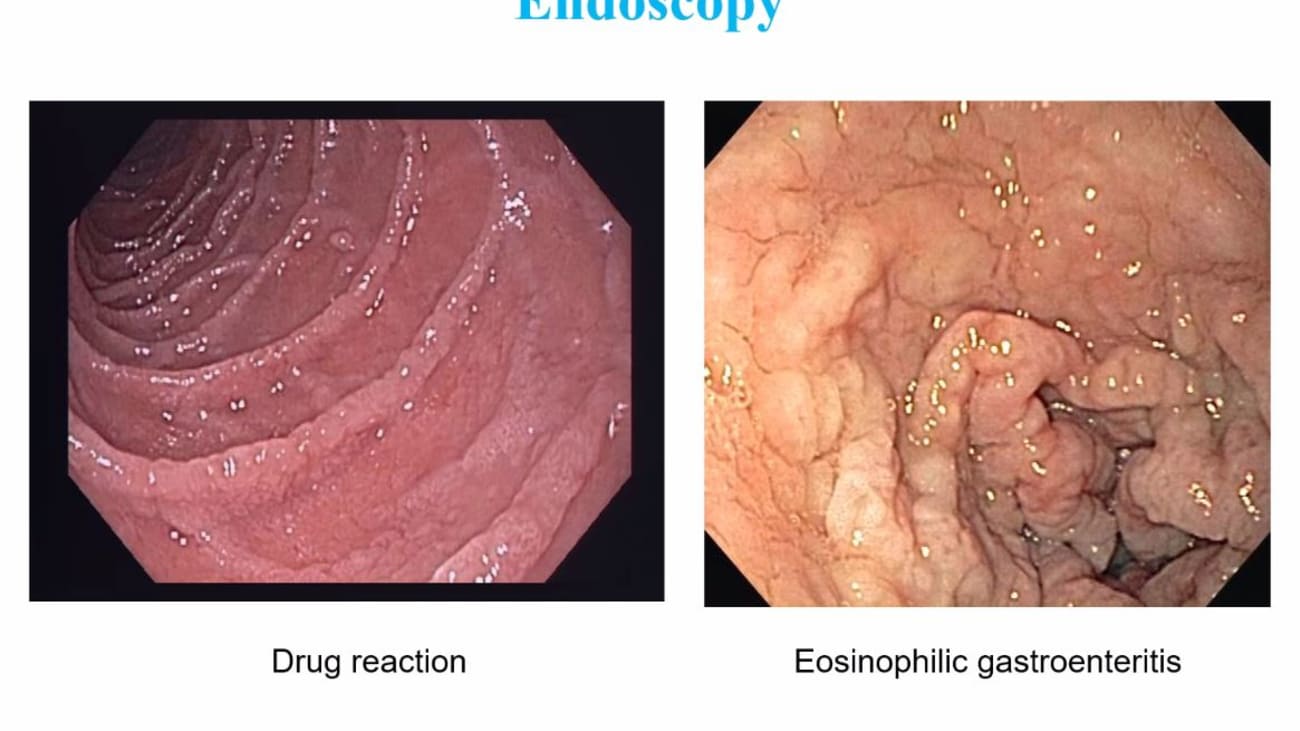
Yeah. Yeah. Hello. All today we will discuss celiac disease before the boards. Celiac disease is a gluten sensitive interim empathy. It's an auto immune disorder that's triggered by gluten which is a complex of water and soluble proteins in wheat, rye and barley and genetically predisposed individuals. When they ingest gluten, it can cause a multi system disorder On the boards. You can get tested for celiac with common manifestations of the disease namely clinical whether it's intestinal an extra intestinal with laboratory abnormalities. How do you test for the diagnosis and of course treatment Celiac disease is pretty common, affecting about 1% of the us population. One in 56 patients will experience gi symptoms and 20% are older than 60 at the time of diagnosis. Here we see a table form serological screening studies of the prevalence across different countries. Classic celiac disease is defined as a patient with malabsorption of symptoms having villus atrophy and biopsy and with the withdrawal of gluten, having subsequent resolution of their mucosal lesions. Clinical signs and symptoms of classic celiac disease include abdominal distention, abdominal pain, anorexia, chronic diarrhea, weight loss and muscle wasting. The picture here on the right if you guessed it is dermatitis or peta for miss, you can have a picture like this on the boards and you would be required to make the connection between this dermatological manifestation of celiac disease. A typical celiac disease is defined as having minor G. I complaints and displaying anyone or many of the following complaints. Whether it's persistent vomiting, chronic constipation or having lab abnormalities like iron deficiency, elevated liver enzymes. even hippo calc mia, Neurological um deficits such as a taxi or neuropathy or epilepsy can be a manifestation of vitamin deficiencies that are also seen instantly. Act disease. For example, b. 12 deficiency. Mhm. Silent celiac disease is defined as a patient who's asymptomatic who's diagnosed with screening serology ease but having no clinical symptoms yet they're histology still displays classic celiac findings such as villus, atrophy or crypt hyperplasia. Lay in celiac disease is defined as having normal vaginal mucosa with minor or no symptoms at one or more time points while on a normal gotten rich diet. A normal mucosa was present earlier in life while ingesting a normal diet and celiac disease developed later. Or a patient was diagnosed with celiac as a child cured with a gluten free diet and then remained asymptomatic with the reintroduction of the gluten rich diet when they were adults. So who should be tested. Anyone with G. I. Symptoms as described prior slide with chronic or recurrent diarrhea, weight loss, malabsorption, even abdominal distention of bloating. Keep in mind that patients who have irritable bowel syndrome. Whether it's diarrhea or mixed should be tested for celiac Other manifestations of the disease as we also described before in terms of liver abnormalities with elevated trans emanates is iron deficiency anemia fully to B. 12 deficiency. Even recurrent feudal law. So short stature you should be testing these patients. Any patient with type one diabetes in other signs or symptoms of Celiac should be tested and the A. C. G. Also recommends asymptomatic first degree relatives of patients with confirmed celiac disease should also be tested. All testing should be performed while patients are on a gluten rich diet. Let's get into some board review questions. Question one A 34 year old woman with a history of I. B. S. Presents as a new patient to your office for complaints of diarrhea for nine months, bloating and abdominal pain. She has mildly elevated Transit Minis is she is interested in treating her I. B. S. Via diet and has read about fog maps and a gluten free diet. You suggest screening for celiac disease prior to altering her diet. What is the most appropriate single next test? Is it a tissue transport tamponnaise I. G. A. Be tissue test with tammy's I. G. See cleared an idea. D. D. Laminated bleedin idea. E. Anti and a musical antibody I. G. A. Or F. H. L. A. D. Q. 28. The answer here is a tissue transfer tamponnaise I. G. A. The testing objective here is serological tests. Let's go over the path of physiology of celiac disease. Gladden is a component of Luton that is ingested in the diet and absorbed by the small intestine. Mhm. TTG is ubiquitous intracellular enzyme that is released by inflammatory and endothelial cells in response to irritation or inflammation. It has the ability to disseminate Gladden this. Delamination produces a negative charge which increases the binding capacity to H. L. A. D. Q. Two or D. Q eight. This potentially stick capacity to stimulate T cells and thus B cells which produces the antibodies, antibodies that have been tested for celiac disease include anti Gladden anti and a museum and anti tissue transport committees as well as antibodies cd emanated. Gladden all of these antibodies are what we're trying to test in serological testing. Now tissue trans contaminates. I. G. A. Antibody is the single preferred test for celiac disease. It has a high sensitivity at 95% and specificity at 97%. There's decreased sensitivity in Children less than two years of age. So they combined testing with denominated leading peptide I. G. A deficiency affects 2 to 3% of celiac patients. So instead of testing for T. T. G. I. G. A you would want to test for T T. G. I. G. Uh Instead the accuracy of T. T. G. I. G. In a patient that has sufficient I. G. A. Is poor 30 to 70%. And so you wouldn't use the I. G. Form in patients who actually have sufficient I. G. A. For testing greed and I G. A. Is an older generation essay that is not sensitive nor specific. This test is really used now Denominated leading peptide idea antibody. It's a newer essay yet its sensitivities only 87% compared with TTG. We would use TTG instead given that it has a higher sensitivity And um easily Ig antibody is a highly specific antibody at 99%. Yet his sensitivity is poor, 79%. It's expensive and operator dependent and is not recommended as first line for screening. Next question, a 55 year old man presents to your office with iron deficiency anemia hemoglobin, 11.5 ferret in his 10. He feels well overall but has complaints of mild fatigue. You schedule him for colonoscopy and upper endoscopy. The colonoscopy is normal without polyps. An upper endoscopy you find that the esophagus stomach and duodenum appear normal. The next best step is a scheduled a patient for a video capsule. Endoscopy Be obtained two biopsies from the second portion of the Duodenum. See obtained six biopsies from the second or third portion of the Duodenum. D obtained multiple biopsies of the duodenum want to tune the ball and four more of the distal duodenum E sensory ology for TTG antibody or F. Sent H. L. A. D. Q. Two A testing. The answer here is D obtained multiple biopsies of the duodenum at least 1 to 2 in the bulb and four more of the distal duodenum. The testing objective here is endoscopic testing. So the endoscopic appearance is celiac disease can vary. It could be a mosaic pattern could be stacking folds scalloping villus atrophy but actually can also be completely normal. You should biopsy symptomatic patients with suspicion of celiac disease. Even with negative serology Biopsy even if it appears normal. And this topic markers have a sensitivity from 15 1994%. Yet a specificity from 92 to 100%. Biopsy should include 1 to 2 from the bulb at the nine o'clock and 12 o'clock positions and four or more from the post bulb. Do Adina Ball biopsies improved diagnostic yield 9-13%. In newly diagnosed patients ball biopsies uncovered villus atrophy, not seen on post blubber biopsies. In 14% of patients with confirmed celiac overall having all these biopsies increases your sensitivity to 96%. As for the other answers in this question, stem a video capsule. Endoscopy may be done in patients who are not able to undergo a G. D. O. Abnormal biopsy. But positive selects ideologies but again wouldn't be your first choice. If you actually have the ability to biopsy the patient sending off T. G. I. G. A would be a good choice but not the next step. When you have the option again to biopsy for disease confirmation. H. L. A. D. Q. Two A testing is helpful when there is discordance between positive biopsy and negative serology is or if a patient is already on a gluten free diet. But again not the next best step here in this question. Marsh classification is something that you may also see in the question stem that you should be familiar with. It characterizes the histological changes in celiac disease. Using the following criteria Increased intra epithelial lymphocytes. About more than 40 per 100 intro sites crypt hyperplasia and villus atrophy. So we see here in this modified marsh classification, it goes from stage zero which is normal mucosa to stage three C, which is total villus atrophy. In between stage one, you will see the increased I yells at more than 40 per 100 insurance sites. By stage two, you'll have some crypt hyperplasia and stages three. Just define how much Phyllis atrophies there from partial sub total to total respectively. Marsh one classification is the most Generalized of the categories you can have lymphocytic diagnosis in patients who do not have celiac disease and it's pretty common in about 5% population. Other causes of March one classification include a big list. As you can see here from H. Pylori to Geo diocese to end said's microscopic colitis and even food hypersensitivity ease. Thus, if you see March one classification, you also want to make sure that patients don't have any other particular causes apart from celiac disease. To cause these changes in the do Adina. Next question which of the following patients would have an increased risk of celiac disease. A patient whose mother has confirmed celiac disease. Be a patient with type two diabetes. See a patient with hypertension. D. A patient with hippolyta academia or E a patient with a sister with breast cancer answer is a patient whose mother has confirmed celiac disease. and the testing objective here is risk factors. Select disease is more common in patients who have first degree relatives with celiac disease. About 10 patients who have Type one diabetes cilia can be found in 3 to 10% of these patients. Also increased risk. Our patients with Down syndrome turner syndrome or Williams syndrome. As for the other answers in this question, stem there is increased risk of select disease in patients with type one diabetes but not type two diabetes. There has been no known increased risk of celiac disease in patients with hypertension, hyper lip oD MIA or family history of breast cancer. So those would not be the right answer. Next question A 43 year old woman presents to your office for further evaluation. She states she has a history of celiac disease for two years but was self diagnosed. No serology or endoscopy ease. She had complaints of diarrhea, fatigue and abdominal bloating. That improved on a gluten free diet. She wants to be officially tested for celiac today. Which of the following test should be done today. A tissue transfer terminates I. G. A. B. Tissue transport terminus I. G. C. And T. And unusual antibody D. D. Laminated lead in I. G. Or G. A. E. An upper endoscopy biopsy or F. H. L. A. D. Q. 28. The answer here is F. H. L. A. D. Q. 28. The testing objective here is celiac serology is on a gluten free diet. So H. L. A. D. Q. 28 R. Is the genetic testing for celiac disease. In patients with celiac, about 95% have H. L. A. D. Q. Two positivity 5% have H. Lady Q. Eight. However, keep in mind that this genetic abnormality is present in 30 to 40% of the population who do not have celiac disease. Thus presence is necessary but not sufficient for diagnosis. It has a very high negative predictive value of greater than 95%. So it's useful in patients in whom the there's uncertainty about the diagnosis and patients whose family members of first degree relatives. For example, if you have a child at risk And those already on a gluten free diet as a patient within this questions them and those that have negative serology ease. But with equivocal, small bowel biopsy results like Marsh one or 2 gluten challenge. You want to perform this. When baseline psychologies are negative and H. L. A. D. Q. Two A. Testing is positive. You want to ask the patient to eat three g of gluten daily for at least two weeks. Diagnostic changes can become evident. At that time, 68% actually had marched three histology and 75% have positive serology is just over a two week period. In one study You want to ask them to eat. For example three slices of whole wheat bread daily and continue that for as long as the gluten challenge is held. If a patient continues to tolerate, you would want to give an additional six weeks of a gluten challenge for a total of eight weeks and repeat the serology at the end of the challenge. Yeah. The other choices in the question stem are incorrect antibodies directed against bleeding or is denominated products or self antigen. TTG are dependent on the ingestion of gluten. So you wouldn't choose those reducing or avoiding gluten in the diet can lead to decreases in the levels of all celiac associated antibodies to normal concentrations, leading to false negative results. After 6 to 12 months of a gluten free diet, 80% of patients, for example will test negative by serology so that wouldn't be helpful for you. These choices would only be better when patients are on a gluten rich diet. Next question, a 67 year old woman with a history of abnormal liver function tests is newly diagnosed with celiac disease by positive serology. An upper endoscopy demonstrating villus atrophy and small bowel biopsy. You suggest a bone density test sending labs for fat soluble vitamins and micronutrient deficiencies. The patient is excited about starting a gluten free diet and already started reviewing several websites. She appears to have a good understanding of the diet. The next appropriate step is a repeat celiac serology in six weeks. Be repeat endoscopy in six months to assess for mucosal healing. See no further follow up needed or d referred to dietitian with expertise and so act disease to discuss a strict gluten free diet. Answer is d you want to refer these patients to an expert dietician and the testing objective here is post diagnosis management. So gluten free diet is the only effective treatment facility at disease. Untreated celiac is associated with an increased prevalence of micronutrient deficiencies. As we discussed before, namely iron, folic acid, vitamin D, vitamin B 12, copper, zinc and carnitine compliance with a gluten free diet is improved in those who see a registered dietitian trained in celiac disease. The other answers and the questions them were wrong. A decrease in baseline values is expected within months of strict adherence to a blue free diet. Current recommendations are to repeat the serology is that the first follow up visit in 3-6 months, not six weeks. Endoscopy should be repeated with biopsies from monitoring cases with lack of clinical response or relapse of symptoms, not for assessment of mucosal healing. So that wouldn't be correct. And all patients with celiac disease should be followed for assessment of symptoms as well as response and adherence to gluten free diet. Next question. 44 year old woman with a history of celiac disease for the past year. Presents your office with continued complaints of diarrhea and fatigue. She reports good compliance with a gluten free diet. You review her initial records and noticed she was diagnosed with biopsy showing March three B. And positive celiac serology ease her exam is normal and stool is negative for a cold blood. The next appropriate step is a repeat celiac serology and visit with a dietician. Knowledgeable about celiac disease. Be video capsule endoscopy. See upper endoscopy with biopsy. D. Colonoscopy with biopsy or e strictly designated nine mg daily for refractory celiac disease. The answer here is a repeat the celiac serology and visit with a dietician. And the testing objective here is evaluation of nonresponsive celiac disease. Nonresponsive celiac disease or N. R. C. D. Is defined as persistent symptoms, signs or laboratory abnormalities. Despite 6 to 12 months of a gluten free diet, It is very common, affecting 7-30% of celiac patients and the most common cause is inadvertent gluten ingestion. This was seen in an old study, we're looking at nonresponsive celiac patients and gluten contamination was found and close to 50% of these patients. Keeping in mind that if patients do have diarrhea, you want to check for microscopic colitis as this came back close to a second cause of non responsiveness, especially if diarrhea is present. So in all patients whom you think are nonresponsive celiac patients. You want to review and confirm the accuracy of the celiac disease diagnosis. In our question stem, it was reviewed that she was diagnosed with biopsy and her serology is were actually positive. The next step you wouldn't want to do is you want to repeat those serology is and you want to assess their adherence to a gluten free diet. If they have poor gluten free diet adherence a scene here on the right, you don't want to get them counseling with a dietician or referrals to a support group and regular follow up with that dietician. If the patient is deemed to have a good gluten free diet adherence while then you'd want to repeat the upper endoscopy with biopsy and if they have diarrhea, definitely get a colonoscopy with biopsies to rule out microscopic colitis. If on those biopsies that enteritis and villus atrophy is present while, then you'll have to exclude other ideologies of villus atrophy, of which there are many. So aside from celiac disease causes of those atrophy can range from having giardia, tropical spruce, bacterial overgrowth, even Crohn's disease, tuberculosis, or even possible medications such as michael Fennelly. Almost certain the endoscopy on these patients are indistinguishable between these differential diagnoses. So drug reaction can look similar to a patient who has is in a Philip gastroenteritis. So going back to the question stem we see here that the other choices are wrong, answers A B and C would be reasonable after confirming the accuracy of the celiac disease diagnosis and inherently gluten free diet. And more information would be needed before you could diagnose this patient with refractory celiac disease and giving them be designated. So that would not be your next step. So, going towards refractory celiac disease, it's defined as persistent or recurrent malabsorption of symptoms along with signs of villus atrophy. On a verified gluten free diet from more than 12 months ideology is unknown prevalence in some studies is about 7 to 8% of these patients With a cumulative incidence of 1.5 at one North American referral center. This diagnosis is based on the immuno final type of the intra epithelial lymphocytes. In patients with refractory celiac disease, you want to check to see whether or not they have abnormal or clonal intestinal T. Lymphocytes. If the answer is no, then they probably have type one refractory celiac disease, but the normal phenotype and that prognosis is much better then Type two. If they are found to have abnormal finna types or the presence of a clone, they have a very poor prognosis of type two. Refractory celiac disease, in which 60 to 80% can develop enter apathy associated T cell lymphoma within five years. And your apathy associated T cell lymphoma is a very rare G. I tract lymphoma, making up about 5% of G. I tract lymphomas. Um As a diagnosis, The most common side is the June um and the median age of diagnosis is 60. There are two types with Type one being the most common at 80 to 90% and is associated with celiac disease patients at that time can present with obstructive G. I symptoms requiring surgical resection, the treatment usually high dose chemo and autologous stem cell transplant. Five year survival Is about 8-20% in patients who come in with refractory celiac disease, type two who developed this type of lymphoma. Strict adherence to a gluten free diet is the only way to help prevent interrupt the associated T cell lymphoma. So what are the 10 things every G. I should know about celiac disease? Well, number one T T. G I. G. A. Is the best serological tests for the detection of celiac disease. Number two, it can be recognized. Endoscopic Lee. Water immersion may help, but normal appearance of the small intestine does not preclude the diagnosis. Number three. To maximize diagnosis, you want to take four biopsies in the second portion of the duodenum and two bulb biopsies at the nine and 12 o'clock positions. Number four, Consider testing. First degree relatives. Those who have a personal history of Type one diabetes downs Turner's or William syndromes. Those with other manifestation of celiac for example, osteoporosis or even iron deficiency or abnormal chemistries. Number five patients on a prolonged gluten free diet should be tested for H. L. A. D. Q 28 genetics. To avoid further evaluation. Number six, basic treatment is a strict lifelong gluten free diet enabled by an expert dietician. Number seven, newly diagnosed patients should be assessed for bone density geometry, fat soluble deficiencies and micronutrient deficiencies. No eight. All patients diagnosed should have clinical follow up to ensure response and adherence to a gluten free diet. Number nine, in persistent or relapsing symptoms, confirm your original diagnosis, review for good exposure and perform a systemic evaluation. If warranted. And number 10 evaluate those with refractory disease for possible malignant transformation. Thank you.